Understanding Baby Loss: A Comprehensive Guide
Published on: 11/02/2025
Welcome to MAMA Academy’s in-depth guide on baby loss. We understand how overwhelming and heart-breaking it can be to navigate the emotional and physical aspects of losing a baby. We have created this resource to provide clear, compassionate information and guidance. You’ll find details on types of baby loss, causes, physical and emotional recovery, as well as crucial support options.
Table of Contents
- What Is Baby Loss?
- Molar Pregnancy
- Miscarriage
- Termination for Medical Reasons (TFMR)
- Telling Others About Your Loss
- Physical Recovery After Early Pregnancy Loss or Termination
- Physical Recovery After Later Loss, Stillbirth, or Neonatal Death
- Contraception After Pregnancy Loss or Birth
- Baby Loss Support
- How to Support a Friend Through Baby Loss
- Returning to Work
- Investigations After Pregnancy Loss or Baby’s Death
- MAMA Pregnancy Helpline
- Further Resources & References
1. What Is Baby Loss?
Baby loss refers to the death of a baby at any stage of pregnancy or shortly after birth. This can include:
- Miscarriage (loss before 24 weeks)
- Stillbirth (loss after 24 weeks)
- Neonatal death (loss within the first 28 days of life)
- Pregnancy complications such as molar pregnancy or ectopic pregnancy
2. Molar Pregnancy
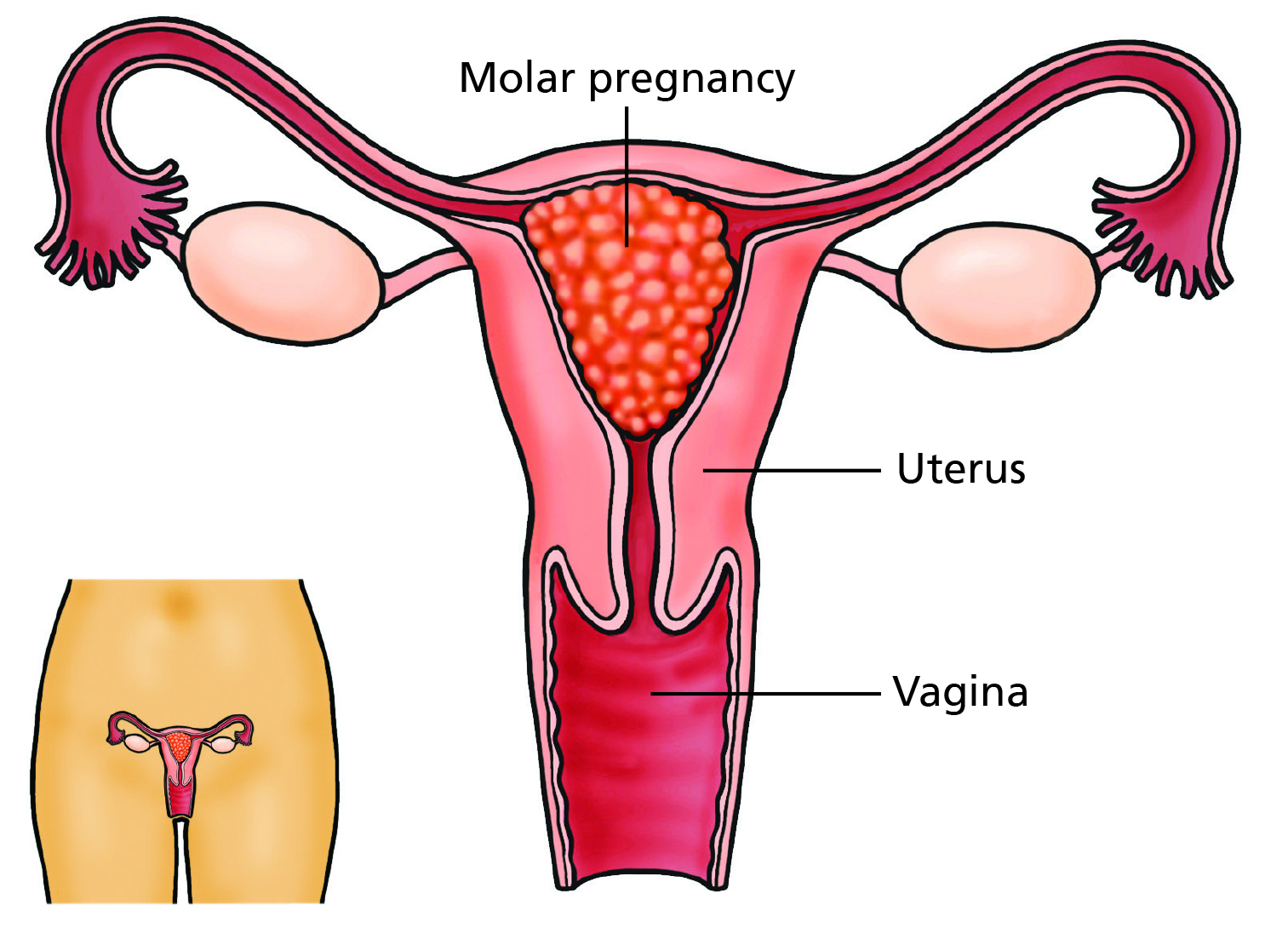
What Is a Molar Pregnancy?
A molar pregnancy (hydatidiform mole) occurs when an abnormal fertilized egg implants in the uterus. Instead of forming a healthy placenta, these cells grow rapidly and take over the uterus, leaving no viable embryo.
Signs and Symptoms of Molar Pregnancy
- Missed periods and a strong positive pregnancy test
- Severe nausea or vomiting
- Irregular bleeding, possibly with fluid-filled cysts resembling tiny grapes
- Uterus larger than expected for dates
- Rarely, high blood pressure and protein in urine
Causes of Molar Pregnancy
Molar pregnancy is typically a random occurrence with no known underlying cause or risk factors.
3. Miscarriage
What Is Miscarriage?
A miscarriage is the loss of a pregnancy before 24 weeks. It is relatively common, with 1 in 4 pregnancies ending in early miscarriage (before 14 weeks) and 1 in 100 ending in late miscarriage (14–24 weeks).
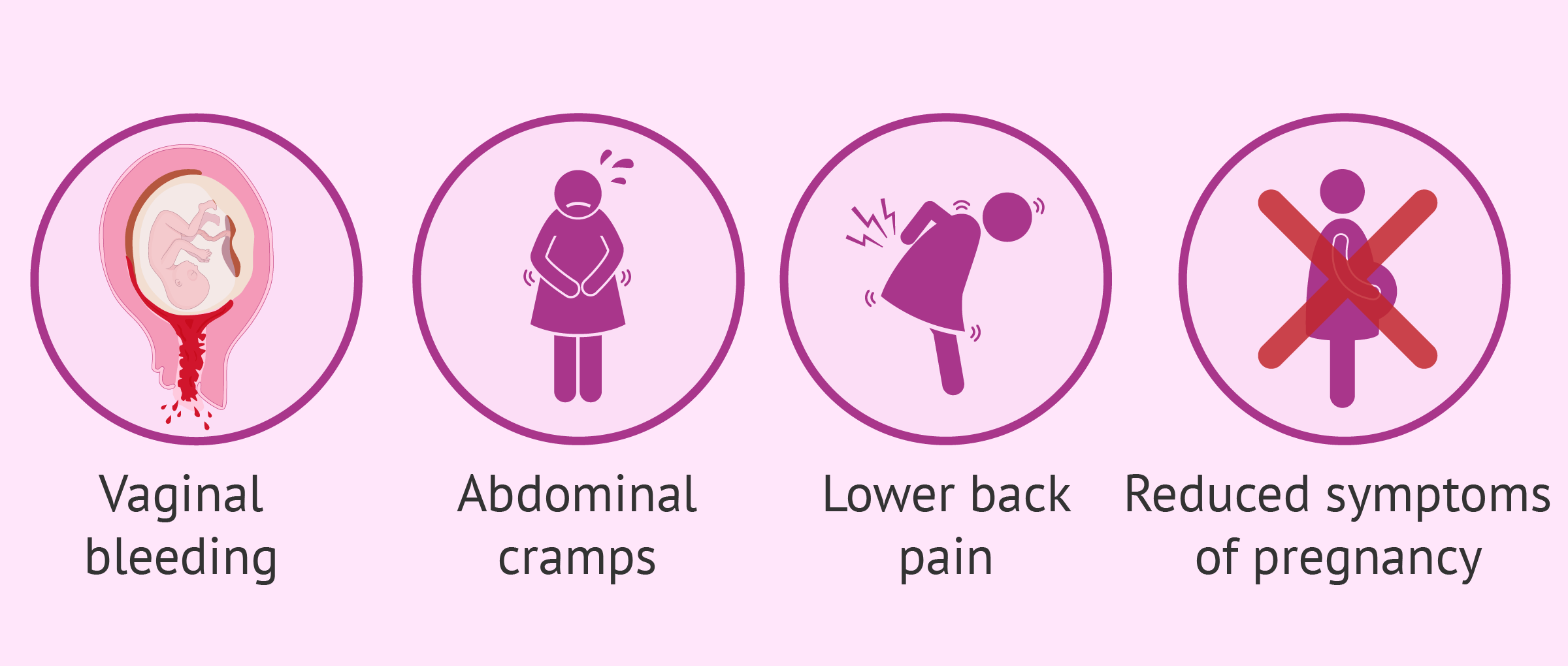
Symptoms of Miscarriage
- Spotting or bleeding
- Abdominal pain
- Possible leaking of amniotic fluid (in late miscarriage)
Causes of Miscarriage
Many miscarriages remain unexplained, though over half are linked to genetic issues. Other causes include:
- Hormonal imbalances
- Blood clotting disorders
- Infections (toxoplasmosis, chlamydia, listeria)
- Diabetes or liver disease
- Fetal developmental problems (e.g., spina bifida)
4. Termination for Medical Reasons (TFMR)
What Is TFMR?
Termination for Medical Reasons (TFMR) may be offered if a baby is found to have a serious genetic or structural condition or if pregnancy complications pose a severe risk to the mother’s health.
When TFMR Is Not Offered
Sometimes, healthcare professionals will detect a condition during a scan but will not suggest termination if they do not believe it to be life-limiting. If you feel the condition is life-limiting or are unclear, you can:
- Ask for a second opinion
- Consult your GP if you’re under 23 weeks 6 days pregnant
- After 24 weeks, the law becomes stricter and ending a pregnancy can only be offered if two doctors believe there is a grave risk to the mother’s health or a substantial risk of the baby being born with serious disabilities.
5. Telling Others About Your Loss
Breaking the news of baby loss can be very difficult, especially if loved ones were excited about your pregnancy. You may feel overwhelmed if you have many people to tell. Here are some tips:
- Put Yourself First: You deserve support.
- Keep It Simple: Share as much or as little as you’re comfortable with.
- Talk as Much or as Little as Needed: Some people find talking therapeutic; others need time.
- Be Prepared for Insensitive Comments: Most people mean well; they may just not know what to say.
- Consider Non-Face-to-Face Methods: Email or text can be easier.
- Let People Know What You Need: If they offer help, accept if you can.
- It Will Take Time: Give yourself and others time to process.
6. Physical Recovery After Early Pregnancy Loss or Termination
Physical Recovery
Recovering physically after an early pregnancy loss or termination is different for every individual. Common aspects of recovery include:
- Bleeding and Discharge: Heavier bleeding at first, then spotting for up to four weeks. Avoid tampons and swimming to reduce infection risk.
- Cramping: Common as the uterus contracts back to normal size.
- Pain Relief: Ibuprofen or paracetamol can help. Consult a healthcare provider if pain is severe.
- Breast Changes: Breasts may feel tender or swollen. A supportive bra or cold compresses can help.
- Follow-Up Care: Usually, you’ll be advised to take a pregnancy test in about 3 weeks. If bleeding worsens or you’re concerned, contact your GP or early pregnancy clinic.
Emotional Recovery
Grief and sadness are common emotions following an early pregnancy loss or termination. Emotional recovery varies for each individual, but the following may help:
- Talk to Someone: Sharing your feelings with loved ones or a support group can help.
- Understand Hormonal Changes: Hormones can intensify emotions, so be gentle with yourself.
- Seek Professional Support: A therapist or counselor can provide guidance and coping strategies.
Practical Considerations
- Rest and Nutrition: A balanced diet and adequate rest can aid in recovery.
- Returning to Work: Take time to recover before resuming work; consider speaking to HR for support.
- Future Pregnancies: If you’re planning another pregnancy, seek guidance from a healthcare provider.
Signs to Seek Medical Help Urgently
If you experience any of the following symptoms, seek immediate medical attention:
- Excessive bleeding (soaking a pad an hour for several hours)
- Severe pain not relieved by medication
- Fever over 38°C (100.4°F)
- Foul-smelling discharge
- Severe depression or thoughts of self-harm
- Difficulty breathing or chest pain
7. Physical Recovery After Later Loss, Stillbirth, or Neonatal Death
Physical Recovery
Recovering physically after a later loss, stillbirth, or neonatal death can take time and varies for each individual. Common aspects of recovery include:
- Bleeding (Lochia): Postpartum bleeding can last up to six weeks. Avoid tampons and swimming.
- Uterine Contractions: More intense if you’ve previously given birth.
- Pain Relief: May be prescribed, especially after a cesarean section.
- Breast/Chest Engorgement: Wear a supportive bra, use cold compresses, or speak with a healthcare provider about medication to suppress milk production.
- Perineal Care: If you had stitches, keep the area clean and report any pain or unpleasant smell.
- Caesarean Section: Recovery may take ~6 weeks. Watch for infection signs (fever, unusual discharge).
Emotional Recovery
The grief following a later loss, stillbirth, or neonatal death is often profound. Some helpful considerations include:
- Seeking Support: Professional counseling and bereavement groups can be helpful.
- Allowing Grief: Grieving is personal and does not have a timeline.
- Communicating with Partners: Grief impacts everyone differently; open communication helps.
Practical Considerations
- Rest and Nutrition: Essential for both physical and emotional healing.
- Work and Activity: Take time before returning to normal routines.
- Future Pregnancies: Consult your healthcare provider about planning for future pregnancies.
Signs to Seek Medical Help Urgently
If you experience any of the following symptoms, seek immediate medical attention:
- Excessive bleeding (soaking a pad an hour for several hours)
- Severe pain not relieved by medication
- Fever over 38°C (100.4°F)
- Foul-smelling discharge
- Severe depression or thoughts of self-harm
- Difficulty breathing or chest pain
8. Contraception After Pregnancy Loss or Birth
After pregnancy loss or birth, you can become pregnant again quickly (as soon as two weeks after a loss/birth). It’s essential to consider your physical and emotional readiness before trying again.
Contraceptive Options
- Barrier Methods: Condoms and diaphragms provide immediate protection.
- Hormonal Contraception: Includes the pill, patch, injection, and implant. Can be started soon after pregnancy loss.
- Intrauterine Device (IUD): Can be fitted by a healthcare provider within a few weeks.
- Natural Family Planning: Requires tracking ovulation but is less reliable immediately after pregnancy.
Considerations for Choosing Contraception
- Physical Recovery: If you had complications, consult your doctor before choosing a method.
- Emotional Readiness: Grief can affect decision-making, so take time before planning another pregnancy.
- Medical Advice: Speak to a healthcare provider to discuss the best options for your health and future family plans.
9. Baby Loss Support
We offer our sincerest condolences if you have lost a precious baby. The impact of baby loss is profound, and you are not alone. There are many organizations ready to support you through your grief.
Choices in Hospital
Even amidst the heartbreak, you still have decisions you can make about your birth experience:
- Pain relief options, water birth (if appropriate), skin-to-skin contact, umbilical cord cutting, etc.
- Accepting or declining medication to stop breastmilk production.
- Possibly donating breastmilk if you feel it’s right for you.
- Counseling may be beneficial and is often available through your maternity unit’s bereavement midwife or external resources like our maternity directory that you can access here.
Making Memories
Your midwives can guide you in creating precious memories:
- Cuddle Cot: Allows more time with your baby in the hospital.
- Memory Box: Often includes items like inkless prints, clay imprints, and keepsakes.
- Photographs: Many parents cherish photos with their baby and family.
- Bathing and Dressing: Discuss options with your midwife.
- Keepsakes and Jewellery: Some families keep a lock of hair or ashes in a piece of jewelry.
10. How to Support a Friend Through Baby Loss
Supporting a friend through baby loss can be difficult, and you may not always know the right thing to say or do. Here are some ways you can help:
- Acknowledge Their Loss: Use their baby’s name if they’ve chosen one.
- Remember Important Dates: The baby’s birthday, due date, and anniversaries can be particularly tough.
- Offer Genuine Help: Instead of saying “Let me know if you need anything,” offer specific help, like cooking meals or running errands.
- Respect Their Emotions: Understand that grief is complex, and your friend may have good and bad days.
- Be Mindful If You’re Pregnant: It can be painful for them to be around another baby or an expectant mother.
- Check-In Regularly: Even months or years later, let them know you still remember their baby and are there for them.
11. Returning to Work
Returning to work after baby loss can be challenging. Parents often face unique emotional and practical difficulties in resuming their professional responsibilities. Consider the following:
Flexible Arrangements
- Explore options such as part-time work, remote work, or phased returns.
- Speak with your employer about compassionate leave policies.
Communicating with Colleagues
- Consider sending an email ahead of your return to explain your situation.
- Let colleagues know how much or how little you wish to discuss your loss.
Managing Emotional Triggers
- Be prepared for unexpected emotional reactions to conversations or reminders.
- Seek support from HR, a manager, or an employee assistance program.
Self-Care
- Take breaks when needed and allow yourself time to adjust.
- Set realistic expectations and avoid pushing yourself too hard.
12. Investigations After Pregnancy Loss or Baby’s Death
Many parents naturally want to understand why their pregnancy ended or their baby died. Various investigations can provide insights, although sometimes no clear explanation is found.
Post-Mortem Examination (Autopsy)
- Purpose: Examines the baby’s body externally and internally to determine a cause of death.
- Consent Needed: Parents must provide consent, and they can choose a full or limited examination.
- Possible Results: May identify genetic or medical causes, but in some cases, no definitive cause is found.
Placental Examination
- Purpose: Investigates the placenta, umbilical cord, and membranes for infection, inflammation, or circulation issues.
Pre-12-Week Pregnancy Loss Histopathology Testing
- Purpose: Examines tissues and cells to rule out molar pregnancy.
Genetic and Chromosomal Testing
- Purpose: Identifies genetic abnormalities or chromosomal issues (e.g., trisomies).
- Karyotyping: Recommended after three or more consecutive miscarriages.
Blood Tests
- Purpose: Screens for clotting disorders, infections, and autoimmune conditions.
- Antiphospholipid Antibody: High levels can lead to blood clots and placental issues.
Ultrasound/Scans
- Purpose: Reviews structural abnormalities of the uterus or the developing baby.
- Transvaginal Ultrasound: Identifies issues with the cervix or womb.
Perinatal Mortality Review Tool (PMRT)
- Purpose: A structured review of care provided to parents and babies when a baby dies after 22 weeks’ gestation.
- Process: Parents can contribute questions or concerns but do not attend the review meeting. Results may take weeks to months.
13. MAMA Pregnancy Helpline
MAMA Academy’s free pregnancy helpline offers non-medical support for anyone feeling anxious about their pregnancy journey, including:
- First-time expectant parents
- Pregnancy after a previous loss
- Pregnancy following complications or birth trauma
Contact Information
If you need reassurance, you can reach out to our helpline for support.
- Phone: 0203 6428 121
- Availability: Leave a message with your preferred call-back time.
- Support Offered: Our midwife, Kate, will respond to provide guidance and reassurance.
Note: For urgent medical concerns, please contact your midwife, GP, or local maternity unit immediately.
14. Further Resources & References
For additional support and information, the following resources may be helpful:
- MAMA Academy: About Baby Loss
- MAMA Academy: Baby Death Investigations
- MAMA Academy: Priorities Set for Stillbirth Research
- NHS: Causes of Stillbirth
- PubMed Central: Related Research
Baby loss is an incredibly personal and often isolating experience, but you are not alone. Whether you’ve experienced an early miscarriage, a molar pregnancy, a TFMR, a stillbirth, or neonatal loss, caring professionals and support networks are ready to help you navigate this journey.
From practical steps like follow-up care and investigations to emotional support like counselling and memory-making, take each day as it comes. Reach out for support when you need it, and remember that healing—both physical and emotional—takes time.
If you’re looking for reassurance, a listening ear, or just more information, MAMA Academy is here to help guide you through. You’re not alone—reach out, seek support, and take care of yourself.
MAMA Academy – Empowering parents and healthcare professionals to work together for safer pregnancies.